If you accept insurances in your office, dental insurance verification is the most important process you can implement that will prevent future headaches.
With tons of insurance plans and gazillion fee schedules, it can be a nightmare to keep up with patients’ benefit information.
Patients want to know what they’re going to owe and don’t want to move forward with their treatment plans unless your office knows what their insurance will cover and what they won’t.
You’ve all heard from the management gurus that office systems are important. Well today I’m going to cover one of the office systems: dental insurance verification process. Let’s dive right in.
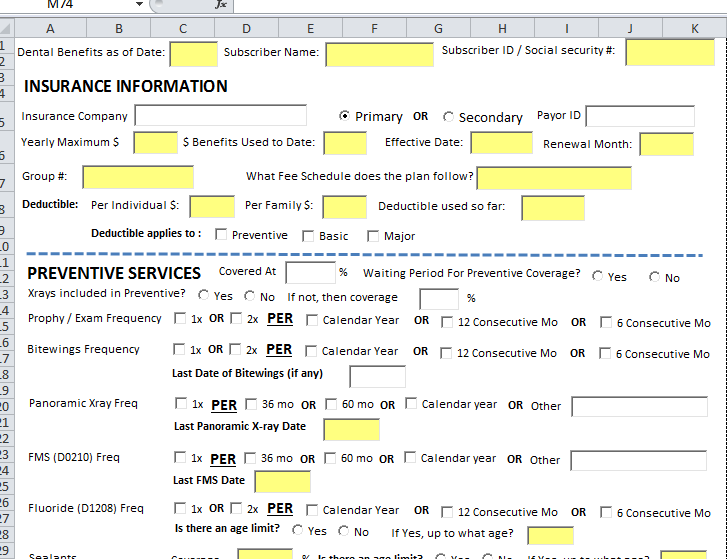
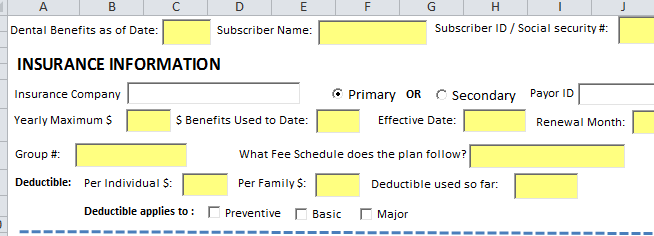
Download our Dental Insurance Verification Template, so you can systematize the verification process in your office.
As I talked about dental office systems in my previous post, Dental Insurance Verification is also a system that you need to implement and tweak over time.
Here’s what you’re going to learn from this post:
- WHY and HOW to do Insurance Verification for patients
- The specific details you NEED to find out to make sure you get PAID
- How to best use the Dental Insurance Verification Template File and AVOID wasting your team’s time over the phone
————————————————————————————————–
Why you should verify patients’ Dental Insurance Benefits
If the scenarios listed below sound familiar-
-
Denial of payment from insurance for a new patient’s preventive visit
-
Denial of payment from insurance for sealants placed on a 10 yr old patient – even though coverage was at 100%!
-
Denial of payment for Scaling & Root Planing – even though there’s 80% perio coverage for a patient with no history of periodontal treatment
-
Payment less than expected from insurance for examination and cleaning visit……
-
Denial of payment for Limited exam / emergency appointment
-
Denial of payment for a recement of a crown on an emergency patient
…then read on…
If anything written above sounds familiar to you, then you’re NOT alone.
I’ve had ALL of it happen to my office. I’m learning from my mistakes and trying to improve the whole insurance process in my office. I’ve now put into place a proper system so these things don’t happen.
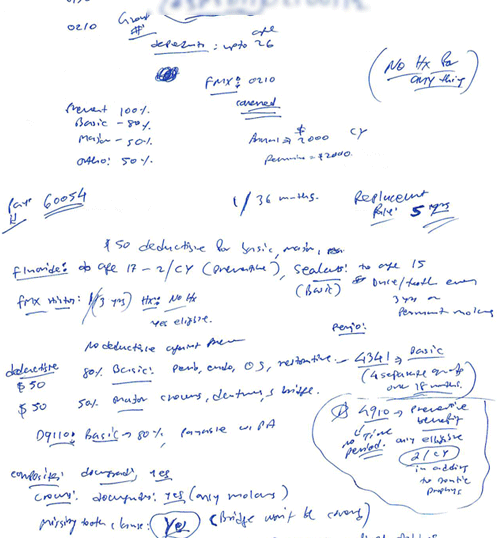
When I first opened the doors to my office, I took lot of the phone calls myself on the days the office was closed. If a new patient with insurance called for an appointment, I would remote log-in to the appointment book to schedule the appointment and immediately get on the phone with the insurance to verify the patient’s benefits.
This is how I did it then….
This is what we’re doing now
- Dental Insurance Verification Template File
Without verifying insurance, there’s no way to know how often the insurance will pay for the patient’s prophy, or if the patient is eligible for x-rays, or if there’s a deductible that applies to their first visit to your office.
If a new patient comes to your office after leaving their previous dentist, there’s no way to know if insurance will pay anything towards their care unless you know they have some dollars remaining in their maximum for the remaining benefit period.
There are several ways to verify patients’ dental insurance benefits:
- In-office Dental Insurance Verification Form:
This is to be filled out by your team by calling the patient’s insurance company.
This is the most comprehensive of all options that gives you all the details you need to know, and it’s also the most time consuming. But more on that later..
- Fax:
Different companies give varying amounts of detail in their faxes. Some provide just an overview with % coverage of different types of procedures (Preventive, perio, endo, os) with no prior dates of history of service.
Prior dates of service are important because you’ll need to know, for example, when the new patient in your office had their last FMX/PANO done, or when they last had Scaling/Root planing done.
- Online Portal:
Some dental insurance companies have an online portal from which you can view information regarding patient benefits and claims.
You should have online accounts for your office for all the insurance companies you’re in-network with. But, don’t rely on this option for all the information.
Only some of the companies show history of services. You also shouldn’t rely on this option for certain stipulations such as waiting periods for scaling & root planing after a general cleaning.
What you can use it for is to do a quick eligibility check if the patient insurance is active for walk-ins.
- Automated services:
These integrate within your practice management software and are not always accurate when it comes to stipulations and waiting periods.
I have never used these, but my colleagues who have used them end up relying on the manual phone call to find out stipulations with certain procedures.
Dentaxchange.com (claimconnect) – service I use for sending claims – You can check for eligibility online by logging into your account. However, it is not detailed and it does not provide stipulations when it comes to perio or prosth work for example.
We’re going to concentrate on the first option for this post, as it’s the option I prefer and have implemented in my office that works well. I ask my team member to request a fax for breakdown of all benefits for all patients when they’re on the phone already verifying information.
Who it’s for:
For Doctors starting out in their practice, I can’t stress how important it is to do this your self just as an exercise so you get to know how insurance works.
I did this myself initially on the days office was closed and made the calls to the insurance companies myself and wrote it all out on paper.
Once I did this repetitively many times over and over again, we came up with the template.
Treatment coordinators and other front desk personnel: If you’re already doing it on the computer and storing it on the network for accessing it from any computer in the office, you’re already on the right track.
The Dental Insurance Verification template is split into different sections. Preventive, Periodontal, Endo, Oral Surgery, Implant services, etc..
Insurance Information
 To make the call to the insurance company: you’ll need
To make the call to the insurance company: you’ll need
- subscriber name,
- subscriber date of birth,
- subscriber ID/Social security
- Your office Tax ID
I won’t go over all the terms here, but I’ll mention some to explain the importance of the terms in regards to insurance verification.
- Dental Benefits as of DATE:
The date you make the initial call to the patient’s insurance should be written here. There are times the benefits do change – either because the patient upgrades the plan or if the insurance decides to change the benefits.
Anytime a change is made to this sheet, the date should be written. If the patient switches insurance, you should create a new template for the same patient with the new insurance plan benefits.
- Benefits Used to Date:
If you get a new patient in your office who has just left their previous dentist in the middle of their benefit period, you will need to know the insurance dollars the patient has used up for the remaining benefit period.
This information can then be updated in your practice management software, so when it comes time for presenting treatment to patient, the correct $ amounts are reflected if treatment cost exceeds the insurance maximum.
- Primary or Secondary Insurance:
It’s important to know whether this is patient’s primary or secondary insurance. Sometimes patients may not even be aware the insurance information they gave you is for their SECONDARY insurance and NOT their primary.
Consider this following scenario to understand the importance
You need to verify with both the patient AND the insurance company whether it’s the primary or secondary insurance.
- Fee Schedule:
There are certain insurances that you may not be aware you’re in-network with, but if those companies follow the fee schedule of a company you ARE in-network with, you can take that insurance.
When I started my office, I got my self credentialed with the most commonly heard insurance companies: Delta, Aetna, Guardian, Cigna, MetLife, etc. But sometimes you’ll get a patient on the phone asking your staff if your office takes their insurance and you’ve never heard of the name.
Don’t automatically assume you’re not in-network and say no to the patient.
Get the policyholder information and provider services phone number, and call the insurance company to find out what fee schedule they follow.
If the insurance company follows the fee schedule of an insurance you’re in-network with, you can let the patient know they’ll have coverage when they come to your office.
For example, first time a new patient called to ask if we take Principal Financial Group insurance, my front desk person did not know as she didn’t see this name in the list of the insurances we have on our website.
After calling the provider services at Principal Financial Group, she found out they follow the Ameritas fee schedule, which we are in-network with. She called the patient back and scheduled an appointment for her as a new patient.
- Deductible:
When asking insurance whether deductible applies or not, make sure to verify whether or not it applies to preventive.
NOTE: For preventive services, some insurances will apply deductible to x-rays and not to exams/cleanings, so make sure to verify this with the insurance.
Most insurances cover preventive services at 100% and deductible will not apply, but there are some who will have a deductible to certain preventive services.
Most patients assume their cleaning/x-rays are covered twice/year at 100%, so make sure to verify this with the insurance to prevent any surprises in the office.
Preventive Services
When it comes to preventive services, verifying frequencies (how often the service is allowed within a benefit period) and history of services is extremely important.
The most commonly used exam codes are 0120 (periodic), 0140 (limited), 0150 (new patient comprehensive).
The template file has check boxes for the common frequencies I’ve encountered so far. Some plans have a separate frequency for 0140 and 0120, which is great, but most plans have a shared frequency among all three exam types – which is usually 2 in a benefit period (calendar year or by consecutive months).
The code D0150 (New patient comprehensive exam) frequency is usually every 3 years per single provider. I’ve also seen every 5 years per provider.
Preventive services count against Maximum? – Since insurances have a maximum $ amount / patient – important to find out if preventive services count against the maximum.
I’ve seen some patients, whose plans allow preventive services to not count against the maximum – which is always an additional benefit to the patient.
X-rays included in Preventive? – Most plans consider x-rays under preventive and if preventive services are covered at 100%, then x-rays are also covered at 100%.
However, some plans have only a 80% coverage for x-rays, but exams/cleanings coverage at 100% – so make sure to verify with the insurance whether or not x-rays are included in preventive and covered at 100%.
Pano/FMX – When calling to verify the insurance, find out the last date of history AND frequency for BOTH the Pano and FMX. Most plans have a shared frequency between Pano and FMX.
Consider this following scenario:
History of Preventive Services for Family Members:
When you’re verifying insurance for a new patient, you should get the history of preventive services for the family members under the same plan.
Make sure to get history (if any) of date of service for last examination they had. For plans that allow exam frequencies of 2 every 12 consecutive months, you should be careful in giving a new patient an appointment for an initial exam or a recall appointment to an existing patient.
Once the appointment is made over the phone for a new patient and you’re calling to verify their insurance, if you find out frequency of 2 every 12 consecutive months, you’ll want to get the dates of history of last two exams (if any on file).
For example: Your front desk schedules an appointment for 4/15/2015 for a new patient. After calling the insurance, she verifies the frequency of 2 exams every 12 consecutive months. The insurance rep informs your front desk of last two dates of history of exams: 11/14/2014 and 5/14/2014. With the frequency limitation of this plan and history of services on file, this new patient is not eligible to receive benefit for an examination until 5/15/2015.
I’ve gotten burned for this in my office. The patient comes in and we know from their plan that preventive services are covered at 100%, so we assume we’ll get paid.
After sending the claim, we get a denial of payment for services rendered for the patient. Because my front desk had assumed 100% coverage for the examination and cleaning and had also informed the patient of it also, we do NOT send a statement to the patient holding them responsible for the payment of services.
This is the financial surprise I always try to avoid to prevent patient leaving the office. I end up writing this amount off for non-payment and move on.
If my team had known and had informed the patient of their out of pocket responsibility BEFORE the appointment, then the patient is held responsible for the non-payment.
Sealants: You should also get the history (if any) of last placement of sealants. Even though coverage may be listed at 100%, you should know if the new 10 year old patient in your chair had sealants placed last year.
Upon clinical examination, you don’t see any sealants on the first molars. You ask mom if the child has had sealants placed. Mom says – “I don’t remember”. History of sealants should be on file for the patient before you let mom know if they’ll owe anything out of pocket.
Basic Services
You may notice on the template I’ve grouped Perio, Endo, Restorative and Oral Surgery under Basic Services. That’s because that is the case with majority of the insurance plans.
However, I’ve come across plans that will have a different coverage for Periodontal services than for Oral Surgery services. For this reason, I’ve created a section for each of the four types of services.
Periodontal Services
Scaling & Root planing (SRP – D4341):
- In addition to the coverage %, you’ll want to find out if there’s any stipulations. Some insurances require the patient to wait 15 days after a general cleaning (prophy) to be eligible for SRP benefit. I’ve learned this the hard way, so make sure this is filled out when verifying insurances.
- Doing all 4 quads in one day: – Some insurances do not allow all 4 quads to be completed in a single appointment, so make sure to have this filled out.
- Frequency & Documentation: Knowing how often the procedure is allowed is important especially if the patient has had history of scaling. Most insurances will require Perio charting and either FMX or PANO, so make sure to have this filled out just in case you don’t have an FMX / PANO on file.
Perio Maintenance: (D4910): Some insurances will allow frequency of perio maintenance visits in ADDITION to prophy frequencies. But for majority, the frequency is shared.
Stipulations apply to Perio Maintenance also. Patient needs to have history of periodontal therapy. Some insurances will dictate how many days you must wait after scaling / active perio therapy, so make sure before you give an appointment for perio maintenance visit, this requirement is satisfied.
Endodontic Services
Some insurances have different coverage % for anterior teeth vs premolars and molars. So make sure to have this filled out!
Crown & Bridge
When getting coverage for crown & bridge, make sure to find out if there’s a downgrade. Many insurances will downgrade D2750 to a D2790 or D2792. Insurance may downgrade all posterior teeth or only the molars, so make sure that’s filled out correctly.
Core buildup (D2950) / Pre-fab Post/core (D2954): Some insurances have a different coverage for post-core and buildups than for restorative or crown coverage, so make sure to find out exactly what it is.
Be careful with Core buildups. Lots of plans are increasingly “bundling” the core buildups and Crowns. What this means is that plans will not pay a separate payment for core buildups.
Aetna, for instance, have increased their documentation requirement to get paid on a core buildup. They want a Pre-op Photo of the tooth (after RCT), post-op photo of the tooth after Core buildup (prior to crown prep), Pre-op Xray and Post-op Xray of the tooth, and a narrative.
After submitting all this, they can still DENY the payment!
Oral Surgery Services
Simple (D7140) vs Surgical Extraction (D7210):
Some insurances have different % coverage for simple vs surgical, so make sure this is filled out.
MUST KNOW: When verifying insurances, find out if patient’s medical insurance needs to be billed first for extractions. That’s why we’ve listed different codes for extractions – some insurances may say for example, for partial bony and complete bony impactions, medical insurance needs to be billed first.
I’ve also seen some plans requiring the medical insurances to be billed first for any surgical extractions (D7210).
More and more insurances are doing this. Problem with this is that patient’s deductible on the medical insurance may be higher than the cost of the extraction(s). If that’s the case, patient will get no benefit from the medical insurance.
Possible solution: Get medical insurance information from the patient. Some plans will accept the ADA dental claim form, but most will require the CMS-1500 (medical claim) form. When medical plan denies payment, send that to the Dental plan.
Implant & Grafting Services
Bone graft D7953 (Bone graft for ridge preservation) vs D4263 (Periodontal bone graft): They’re both different and some insurances cover one and not the other, so make sure to verify this.
Implant Benefits: Implant Placement (D6010), Custom Abutment (D6057), Pre-Fab Abutment (D6056), Implant Crown (D6058 / D6059) – Verify if there are any implant benefits. Some insurance provide no benefits towards placement, but may provide benefits towards implant restoration.
Whenever Implant is treatment planned for an insurance patient, I always send out a pre-determination to the insurance with the following codes: D6010, D6057, and D6058. If there are implant benefits provided by the insurance, your office will know the exactly $ amounts for each service. If insurance will downgrade the D6058 (all ceramic), you’ll know exactly what it is.
Orthodontic Services
When verifying orthodontic benefits, make sure to verify how the benefits are paid. Most insurances do not pay in one lump sum. They will pay periodically, but you need to find out whether or not you need to submit a claim. If the representative states the benefits are paid automatically periodically, you need to find out how frequently the payments will be made.
How to Best Use This System for Time Savings
You may have already noticed the template is comprehensive. Doing it for all new patients who have insurance will quickly eat up a lot of administrative time.
Here are some tips on using the Dental Insurance Verification template:
- When on the phone with the insurance rep, time your self and see how long it takes to go through the file. Track your improvement as you do this repetitively for new patients.
- If a mom calls for an appointment for her son who is 15 – it doesn’t make sense to get implant, oral surgery, perio stipulations, crown & bridge benefits. You should quickly only get % coverage for preventive, basic and major procedures.
- While on the phone, make sure to request fax breakdown of the benefits. This is helpful if you cannot get a rep on the phone right away, so at least you can fill in some of the details from the fax.
- It’s not always possible to verify benefits BEFORE the patient comes in for appointment. For a new patient who is a walk-in, after checking in at the front desk, once patient is in the operatory – a team member should quickly call the insurance and make sure they’re eligible for an exam / emergency exam and request a fax right away.
- Set aside a separate time during the day during downtime to do these calls. If possible, group patients with same insurance plans, so you can do multiple patients during the same call.
- You will develop your own process that works for your office using this system. The template is only meant to organize information. You may add to it or remove details that you find unnecessary for your office.
Some final words…
Even after doing our due diligence to follow up with insurances for patients benefits, there are still times our claims come back with less than expected coverage.
Having this dental insurance verification system in place has significantly reduced problems with getting paid from insurance, but it does take investment of administrative time.
I’m still trying to improve this process further. I hope I’ve covered as much detail needed to help you work through insurance headaches in your office when it comes to verifying patients’ dental insurances.
But we’re only getting started. Continue to tune in for more posts regarding everything insurance related! Feel free to comment below and share if you’ve done things differently. Or maybe you have a question about the process I’ve discussed – let me know in the comment box below.